News Story
Development of Diagnostic Biomarkers for Determination of TBI
The research team spearheading the M-CERSI-funded project “Development of Diagnostic Biomarkers for Determination of Traumatic Brain Injury” is working to enable the characterization of two specific lipid molecules as diagnostic biomarkers of traumatic brain injury (TBI). M-CERSI researchers Maureen A. Kane, Ph.D., Marta Lipinski, Ph.D., Jace W. Jones, Ph.D., Chinmoy Sarkar, Ph.D., Masahiro Iwamoto, DDS, Ph.D. and FDA researcher Chris Leptak, M.D., Ph.D. are collaborators on this project.
Over 200,000 Americans are diagnosed with a traumatic brain injury - brain injury caused by an outside force, like a car accident or sports injury - every year. TBIs are currently diagnosed using a series of eye opening, and verbal and motor response assessments known as the Glasgow Coma Scale. This scale has been used for decades, but its subjective nature often leads to disagreements between medical personnel who administer it.
Scientists have long sought more objective diagnosis alternatives for TBIs. In the past, researchers have investigated the use of protein and RNA as biomarkers (measurable indicators of the presence and severity of disease) for TBI, but these diagnosis methods remain unapproved by the FDA.
Now, M-CERSI investigators say that two specific lipid molecules may have greater diagnostic potential and brain specificity for TBIs.
“We started our collaboration looking at the basic biological connections for brain injuries,” says Kane. “And through those studies, we identified two lipid molecules that were changed after the brain injury, and we thought that these would make good biomarkers. Molecules that make good biomarkers are things that you can measure easily and that change after injury. It is essential that these biomarkers specifically address traumatic brain injuries, particularly instances of polytrauma."
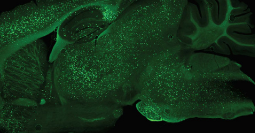
These lipid molecules can be measured in blood plasma and change 24 hours after a traumatic brain injury - so observing them could objectively indicate the presence and severity of TBI.
Unlike other TBI assessments, these lipid molecules can also diagnose TBI if the patient is unconscious or under the influence of alcohol or drugs. Once researchers confirm a cranial injury, they need to determine its severity.
“We want to see how the changes in the biomarkers correlate with the severity of the TBI injury,” explains Lipinski. “And for that, we’re doing both biochemical assessments, like how many brain cells are dying, and we’re also assessing mouse behavior. We’re looking for changes in cognition, memory, and motor function. We know that these things are also affected in human patients with TBI. So it gives us a good readout of the severity of the injury, and we can correlate that with the changes we see in these lipid molecule biomarkers.”
After establishing translational potential for human TBI patients, the team plans to submit a Submission Letter of Intent to the FDA for Biomarker Qualification of these two lipid molecules.
Published March 9, 2021