News Story
Fischell Institute Advances Surgical Innovation for LMICs
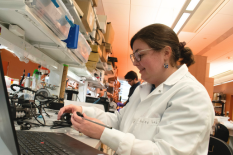
Since 2020, the Robert E. Fischell Institute for Biomedical Devices has partnered with Jenna Mueller, an assistant professor in the Fischell Department of Bioengineering and a Fischell Institute Affiliate Fellow, on her innovative KeyScope device. The KeyScope is a low-cost, durable, and reusable laparoscopic system designed for low- and middle-income countries (LMICs).
Mueller began developing the KeyScope during her postdoctoral research at Duke University, where she collaborated with Tamara Fitzgerald, an associate professor of surgery, research professor of global health, and pediatric surgeon.
The idea for the KeyScope was inspired by Mueller's previous work on the Pocket Colposcope, a low-cost optical device used to diagnose cervical dysplasia in LMICs. After seeing the Pocket Colposcope, Fitzgerald encouraged Mueller to adapt its core technology to create a laparoscope that could be manufactured and used in Uganda. Fitzgerald’s partnerships with hospitals in Uganda were instrumental in shaping the project.
In 2019, Mueller met William Bentley, director of the Fischell Institute, during her interview for an assistant professor position. She was impressed by the institute’s role as an “in-house engineering design firm,” calling it a “gold mine” and an ideal environment to advance the KeyScope project.
Fischell Institute Chief Engineer John Rzasa and Senior Engineer Kevin Aroom then worked to redesign and refine the device. They addressed technical challenges, including developing a specialized camera module, custom-printed circuit board, and waterproof casing. The waterproofing allows the device to be cleaned using Cidex, a disinfectant commonly used to clean medical devices, eliminating the need for autoclaving or gas sterilization, which are often unavailable in LMICs.
“Working on the KeyScope project with Dr. Mueller was a challenging but rewarding effort to integrate small electronics and optics into a custom ergonomic package that expands laparoscopic procedure availability worldwide,” said Rzasa.
Mueller secured funding from the UM Ventures Medical Device Development Fund and the National Cancer Institute. This enabled the team to transition from the KeyScope’s first-generation design to an improved, second-generation device. The team conducted in vivo trials with pigs at Duke University, where Fitzgerald had access to a surgical training lab. These trials paved the way for human clinical trials at the Ugandan Cancer Institute, set to begin in 2025.
“John and Kevin’s insights have been invaluable for this project,” Mueller said. “I don’t think it would be where it is without their help.”
Several members of Mueller’s Global Biomedical Devices lab have contributed to the project over the years, including: Michele Kaluzienski (Mueller’s lab technician), Annie Barnes (BIOE Ph.D.’28), David Garvey (MPower fellow, BIOE M.S.’23), Jason Chen ( MPower fellow, Robotics M.S ’25), Talya Simcox (BIOE B.S’25), Surabhi Singh (Fischell Institute research intern, BIOE B.S.’26), Wilhelm Smith (BIOE B.S.’26), and Tri Quang (postdoctoral research associate).
Mueller’s ultimate goal is to develop a suite of laparoscopic technologies tailored to LMIC challenges and to build local capacity for medical device translation in Uganda.
“My hope is that this technology will help people with cancer and other diseases in low-income communities, while empowering Ugandan engineers to bring medical devices into clinical practice,” she said. “The societal impact on LMICs could be significant.”
With the support of the Fischell Institute, the KeyScope is now closer to transforming surgical care in deprived regions.
Published December 13, 2024