News Story
Voice-activated telehealth technology could strengthen patient-physician connection
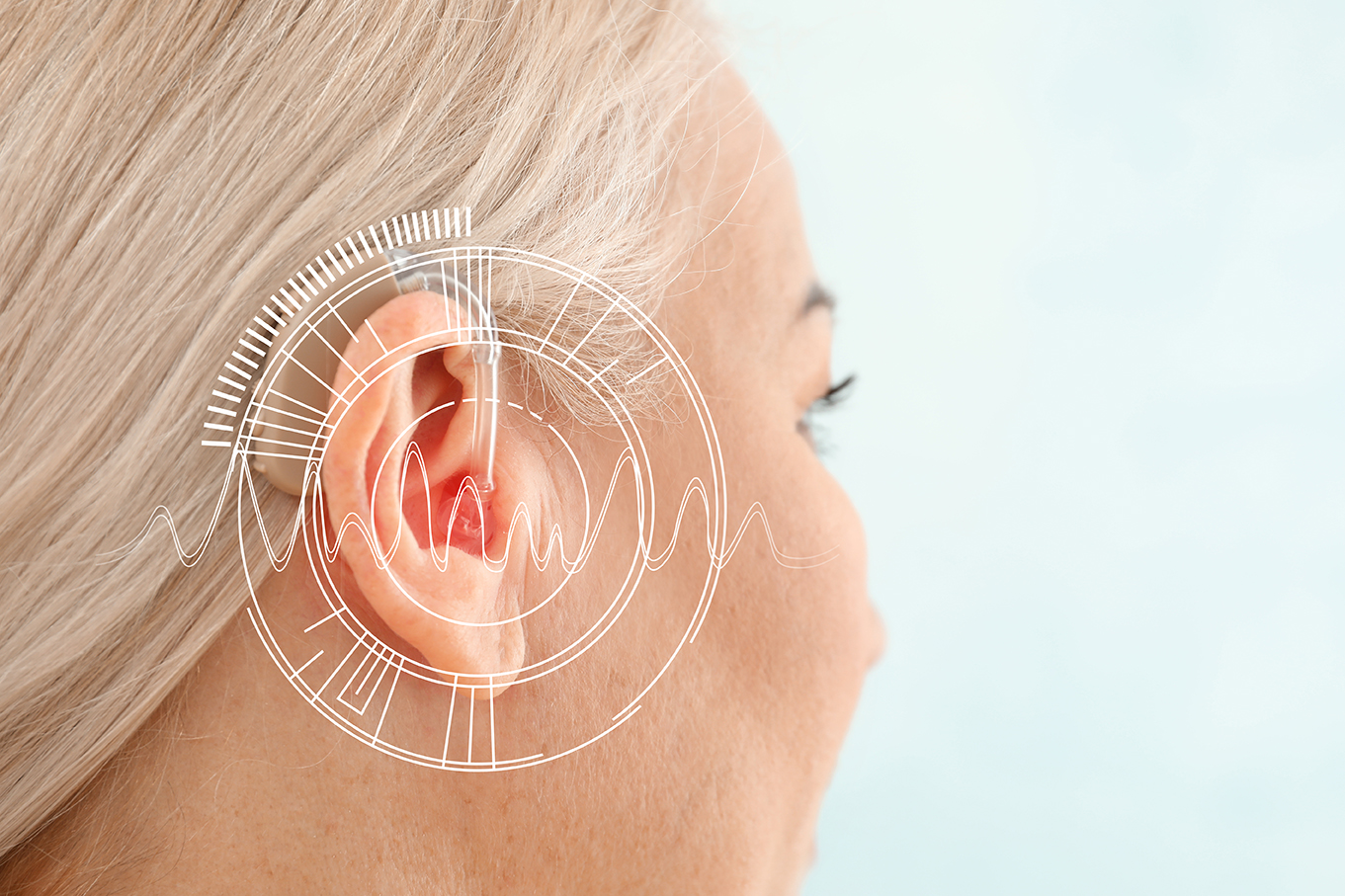
Imagine a world where your smart device checks on you to make sure you’ve taken your medication and alerts your provider with clinically important information. With the increasing popularity of new advances in telehealth, driven in part by COVID-19 safety measures, a team of University of Maryland researchers wants to make this a reality—and strengthen the connection between patients and providers.
Professors Margrét Bjarnadóttir and Bruce L. Golden and doctoral student Lida Apergi in the Robert H. Smith School of Business and Professor John Baras (ECE/ISR) partnered with the MedStar Health Research Institute to analyze the impact and use of a voice-activated telehealth system, exploring patterns between patients with heart failure and the utility of telehealth for patient self-monitoring.
The MedStar team, led by Nawar Shara, director of its Department of Biostatistics and Biomedical Informatics, and including doctors, study coordinators and scientists, focused on heart failure patients because of their requirements to practice self-care and check in with their physicians regularly. Frequent feedback to health care providers about a patient’s compliance and symptoms could be an ideal use for telehealth technology.
“Using telehealth can greatly improve the response time of the provider,” said Shara. “Patients are told to call their provider immediately for certain signs of a worsening condition, but they often don’t. Using a telehealth system that’s enabled by Amazon Alexa, for instance, could help remind patients to take their medication and make sure that they are monitoring their condition as advised.”
In addition to the voice interface used by the patients, the team built a live dashboard that allowed the study coordinator to monitor the patients’ conditions and intervene when needed.
Two groups of heart failure patients were monitored over 90 days. Each group was assigned to a different type of voice interface: the Amazon Alexa voice interface, that only required a patient to speak to use it; or a tablet interface, that required a patient to navigate to an app on a touch screen to get to an animated and voice-enabled avatar.
“Voice-activated technology has the potential to help patients, especially those that have reduced fine motor skills and may have a harder time clicking on apps with their fingers,” said Bjarnadottir. “Studying the two interfaces allows us to compare and contrast two modes of delivery—the Alexa and an avatar on an iPad.”
The research team measured the resulting data against patients’ demographic and clinical characteristics, as well as historical technology usage, and found older patients were more likely than younger patients in the study to use the telehealth technology to manage their conditions. However, they also found that the more medications a patient was prescribed, the less likely they were to use telehealth technology.
“Telehealth is still relatively new, and we are still learning what impacts the adoption of these technologies,” Shara said. “However, we can form hypotheses based on our data. Patients who have multiple prescriptions may feel the need to meet with their doctor directly to discuss different symptoms and side effects, as opposed to interacting with the telehealth technology. Additionally, they may have multiple diagnoses to track.”
The study could be the start of helping to empower patients to take better control of their care, as well as improving accessibility of healthcare to rural and vulnerable populations, the researchers said.
“This research has wider implications for using telehealth to manage other conditions—such as mental health,” said Bjarnadottir. “There are many chronic conditions that require patient self-management. In this research, we have clearly demonstrated that telehealth using voice interface technologies can serve a large role in empowering patients to better manage their health, potentially preventing adverse events such as hospitalizations and emergency department visits.”
— Many thanks to author Laura Hayes of the Robert H. Smith School of Business and to Maryland Today, where this story appeared on April 8, 2021.
Published April 8, 2021