News Story
Jewell Research Lab Explores New Therapies for Treatment of Juvenile Diabetes

Approximately 3 million Americans suffer from Type 1 diabetes (T1D), a chronic condition in which the body does not produce insulin, a hormone needed to get glucose from the bloodstream into the cells of the body.
The body relies on sugar for energy; when a person eats food, the cells in the pancreas – known as beta cells – release insulin into the bloodstream. Then, insulin attaches to cells and signals for them to absorb sugar from the bloodstream.
In cases of T1D – commonly referred to as juvenile diabetes – patients rely on insulin injections to regulate the amount of glucose in the blood and to avoid the effects of hyperglycemia.
While decades of research have led to tremendous improvements in insulin replacement therapy, there is no cure for T1D, and treatment remains a lifelong commitment. Additionally, because many patients are diagnosed with T1D before they reach adulthood, it can be challenging for caregivers to enforce the degree of compliance and lifestyle changes treatment necessitates.
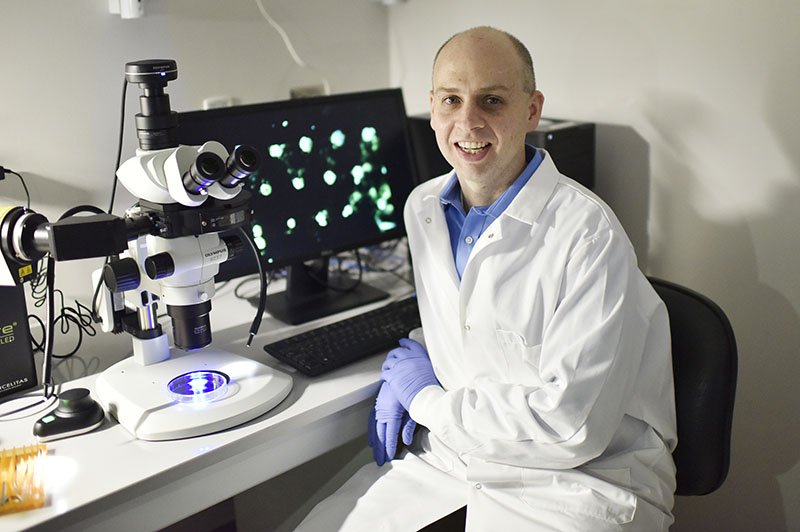
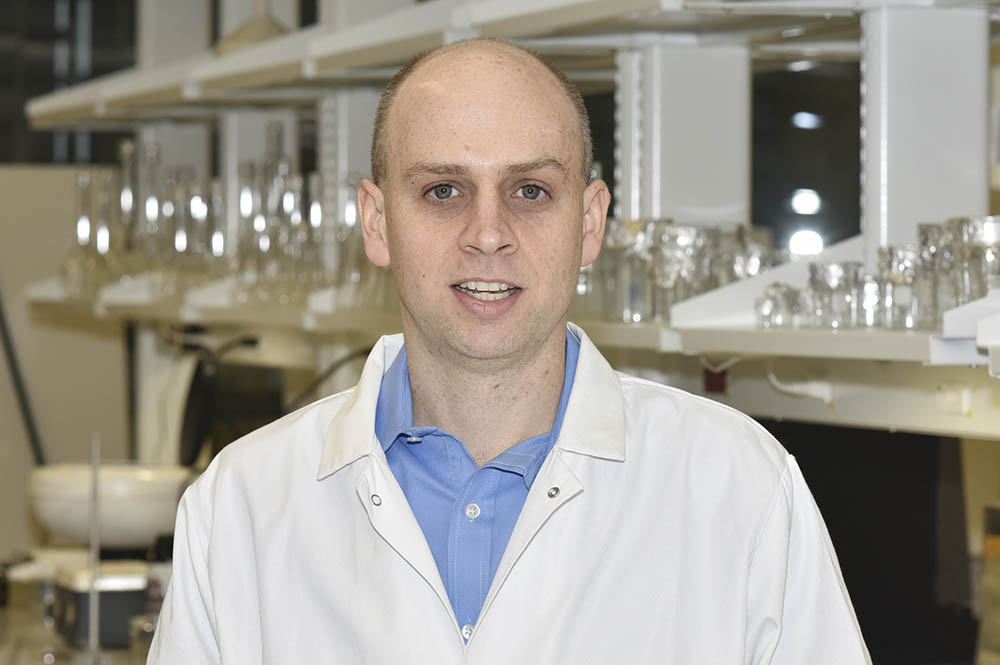
To address these challenges, Fischell Department of Bioengineering Assistant Professor Christopher Jewell and members of the Jewell Research Lab are applying a two-year $500,000 grant from the Juvenile Diabetes Research Foundation (JDRF) to investigate a cutting-edge immunotherapy strategy for T1D.
Arming the Immune System to Fight Diabetes
The human body carries a variety of white blood cells, including what are known as T cells and B cells. Both T cells and B cells are instrumental in building immunity – together, they detect and destroy infected cells and even work to prevent re-infection. In the case of T1D patients, however, self-reactive T and B cells mistakenly identify insulin-producing beta cells in the pancreas as foreign, and in response, they mount a chronic attack.
To wage a counter-offensive, conventional therapies have focused on immunosuppressant drugs – drugs that lower the body’s ability to reject organs during organ transplants. Unfortunately, such therapies can leave individuals immunocompromised and susceptible to new infections because they are broadly acting.
Jewell and his lab have been working to develop new immunotherapies that seek to direct or modulate immune cell populations toward regulatory functions that control inflammation and specifically block self-reactive cells without suppressing healthy immune function. Building on their recent pre-clinical studies, the Jewell lab is working to develop “vaccine-like” therapies capable of generating protective regulatory T cells. Their approach is multidisciplinary, combining biodegradable materials and nanotechnology to engineer the local function of lymph nodes – the tissues that coordinate immune function.
In the lymph nodes, T cells and other immune cells with specific reactivity receive sets of signals that help them develop and expand toward either inflammatory or regulatory cells. In the case of healthy immunity, these cells leave the lymph nodes and migrate to sites of infection; but, in cases of autoimmunity deficiency, these cells leave lymph nodes and directly target the organs that have been attacked. By using unique features of biomaterials to generate these regulatory cells, Prof. Jewell hopes to control autoimmunity with unique specificity, while leaving the rest of the immune system intact.’
“While the existing treatments have provided a lot of gains for patients, current treatments really only provide options to help manage symptoms, without treating the underlying cause of disease,” Jewell said. “Our work – and a number of other exciting immune-based therapies being explored in the field – have the potential to exploit the specificity of the immune system to treat the underlying malfunction that occurs in immune recognition during T1D. Understanding and exploiting this idea could enable next-generation therapeutics that are transformative in realizing an immune-based cure for T1D.”
In addition to applying these techniques to develop new therapies for diabetes, Jewell and his team are advancing the concept of lymph node engineering for application to other autoimmune disorders, including multiple sclerosis.
With support from the JDRF, Jewell will head a team of researchers from his lab and collaborators at the University of Maryland School of Medicine, Dr. Stephen Davis (Chair, Department of Medicine) and Dr. Jonathan Bromberg (Division Head, Transplant Surgery). The team is designing and testing degradable polymer depots co-loaded with self-molecules attacked during T1D and signals that reprogram how immune cells respond to self-molecules after differentiating in lymph nodes. The rationale for this approach includes recent studies showing that co-delivering regulatory signals and self-molecules associated with disease can actually promote immunological tolerance.
While this concept has great potential, the process of getting these self-molecules and modulatory signals to the correct immune cells and tissues – and in the correct combinations and time intervals – is a daunting task.
Still, the team knows that their findings could help change the way autoimmune diseases are treated.
Once Jewell and his team have designed the depots, these carriers will be screened in cell cultures to identify the formulations that best reduce inflammation.
“Using these optimal depots, we will test to see if introduction of these depots reprograms lymph nodes to generate self-reactive cells that are regulatory instead of inflammatory, hopefully in a manner that prevents, stops, or even reverses diabetes in the two pre-clinical models in which our studies will be carried out,” Jewell said.
If successful, the team’s research could help engineers, scientists, and clinicians understand the role of specific therapeutic components in designing new T1D therapies. With the JDRF’s strong translational network, the team will also have connections to support translation of new treatment options that integrate the concept of locally programming the environment of lymph nodes with controlled release depots for stronger and more selective T1D therapies.
Published August 2, 2016