News Story
UMD Researchers Pioneer Improved Photoimmunotherapy Treatment Against Metastatic Cancer
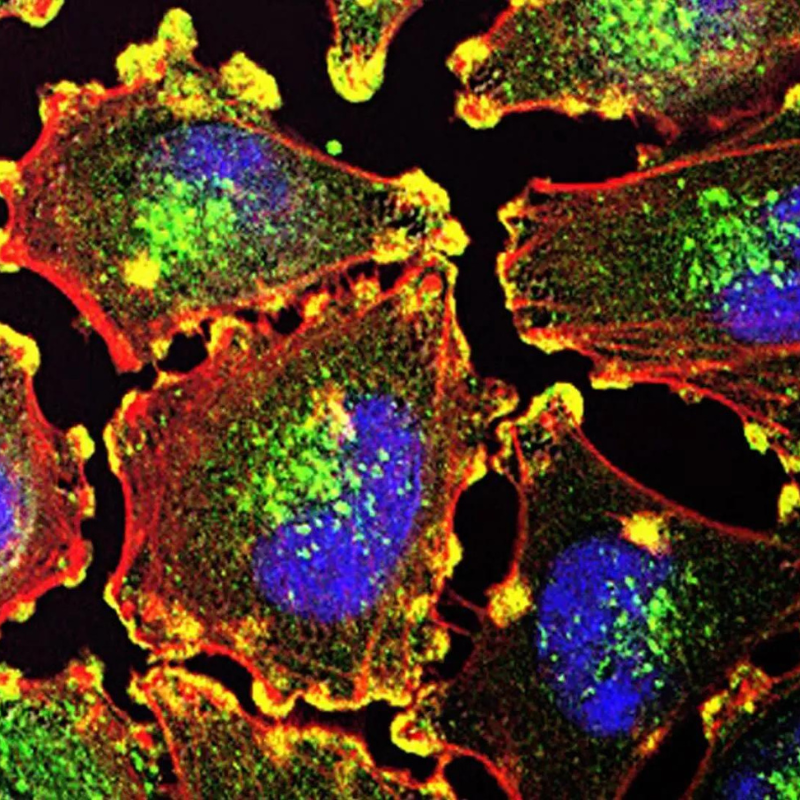
Photo courtesy of the National Institutes of Health
A team of researchers from the Fischell Department of Bioengineering (BIOE) at the University of Maryland has made new strides in the fight against metastatic cancer, for the first time successfully combining three cutting-edge photoimmunotherapy technologies to help prevent the spread and return of the disease, while minimizing illness and other familiar side effects of cancer treatment.
The study, published in Science Advances, is a collaboration between the University of Maryland and Modulight, a designer and manufacturer of lasers for medical application.
Using mouse models, the team studied advanced forms of the deadly disease, which in humans has an average five-year survival rate of less than 30%—a statistic that has not changed significantly in the past 30 years. Many patients relapse due to residual lesions smaller than a millimeter that remain after initial treatments. These micrometastases are difficult to detect, often develop resistance to standard treatments, and are the root cause of metastatic cancer.
A rising method of treatment, photoimmunotherapy targets cancer cells with microscopic, nano-engineered cancer drugs that are activated at the site of lesions using laser light. But because of widely varying responses to the treatment from person to person, the treatment often relies on trial-and-error drug delivery, and moreover, no method can readily monitor whether the drugs were delivered effectively or had the desired therapeutic effect.
As the UMD–Modulight study demonstrates, a combination of targeted “photo(nano)medicine,” imaging, and monitoring of treatment responses could in the future overcome these challenges, achieving better treatment outcomes and predicting tumor response.
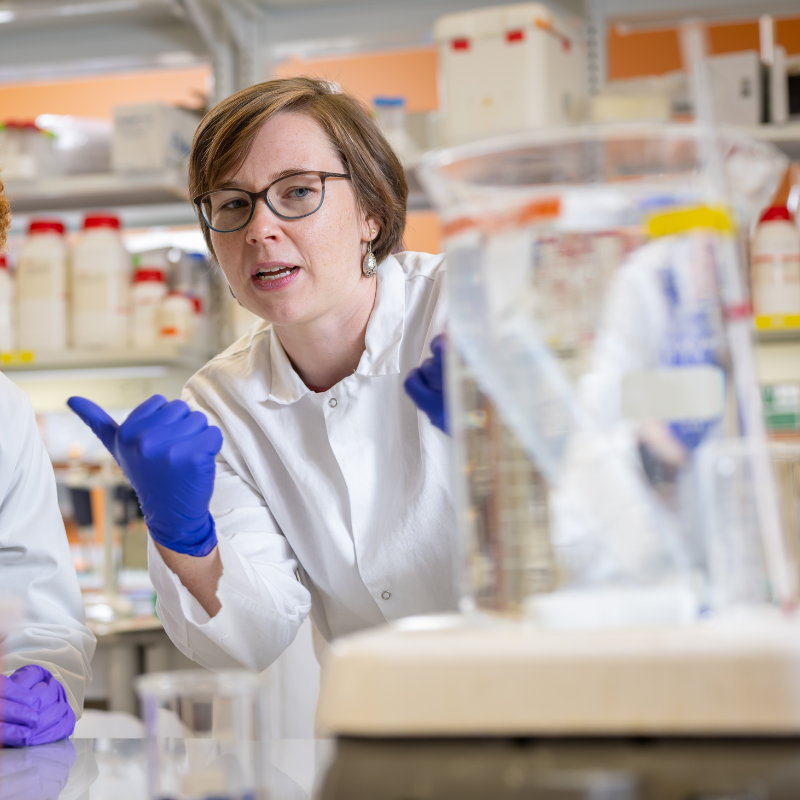
“Patients undergoing cancer treatment exhibit varying tolerances and individualized responses. Through continuous monitoring of their progress, we can promptly determine if treatment adjustments are needed while they are actively receiving care," said study leader Huang Chiao Huang, Associate Professor of bioengineering. "There is no need to postpone decisions until the next scheduled session,” .
The goal is to minimize the number of treatment cycles required while minimizing burden on the patient's body, in contrast to conventional treatment approaches.
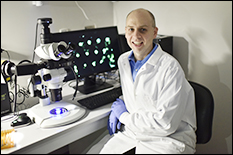
Dr. Huang Chiao Huang
The approach relies on the combination of three advanced technologies to improve treatment outcomes.
- Targeted Photo-Activable Multi-Agent Liposome (TPMAL): The specialized drug delivery system designed by the UMD research team involves tiny lipid-based containers, or liposomes, loaded with chemotherapy drugs containing fluorescent markers that allow researchers and doctors to track the liposomes as they move through the body to precisely target cancer cells.
- Laser Endoscopy (ML7710): ML7710 is a high-tech, laser-assisted camera created by Modulight that uploads information to the company’s servers to analyze in real time the different colors of light emitted by TPMAL inside the body.
- Fluorescence-guided intervention: That information gathered by ML7710 allows doctors to determine how well the drug carriers are reaching and delivering their cargo to metastatic cancer sites, as well as calculate the precise amount of laser light needed during photoimmunotherapy, minimizing tissue damage.
“This approach ensures that the treatment remains both effective and uniform,” said Huang, who leads the Optical Therapeutics & Nanotechnology Laboratory. “This process is repeated as necessary for each patient, resulting in a personalized dosage tailored to maximize treatment effectiveness within a single session.”
When these three technologies are combined and applied in mouse models with peritoneal carcinomatosis—a type of cancer that can be caused by spreading ovarian cancer—the research team observed remarkable improvements. The TPMAL system enhances drug delivery to metastatic tumors, while sparing normal tissues. Furthermore, the ML7710 system monitors the TPMAL drug in real time and customizes light dosimetry for each patient.
The research team is working to establish a comprehensive panel of biomarkers that would allow doctors to promptly determine the optimal dosage for each patient during a treatment session.
“The goal is to minimize the number of treatment cycles required while minimizing burden on the patient's body, in contrast to conventional treatment approaches,” Huang said.
Other authors of the study included BIOE graduate students Barry J. Liang, Sumiao Pang, Chen-Hua Ma, Brandon Gaitan, Aaron J. Sorrin and Idrisa Rahman; BIOE postdoctoral associate Payal Srivastava; BIOE undergraduate Nada Fadul ’24; and Dana M. Roque, an associate professor of obstetrics, gynecology and reproductive sciences at the University of Maryland School of Medicine at the University of Maryland, Baltimore.
Published October 25, 2023