News Story
On A Mission to Bridge the Global Health Gap

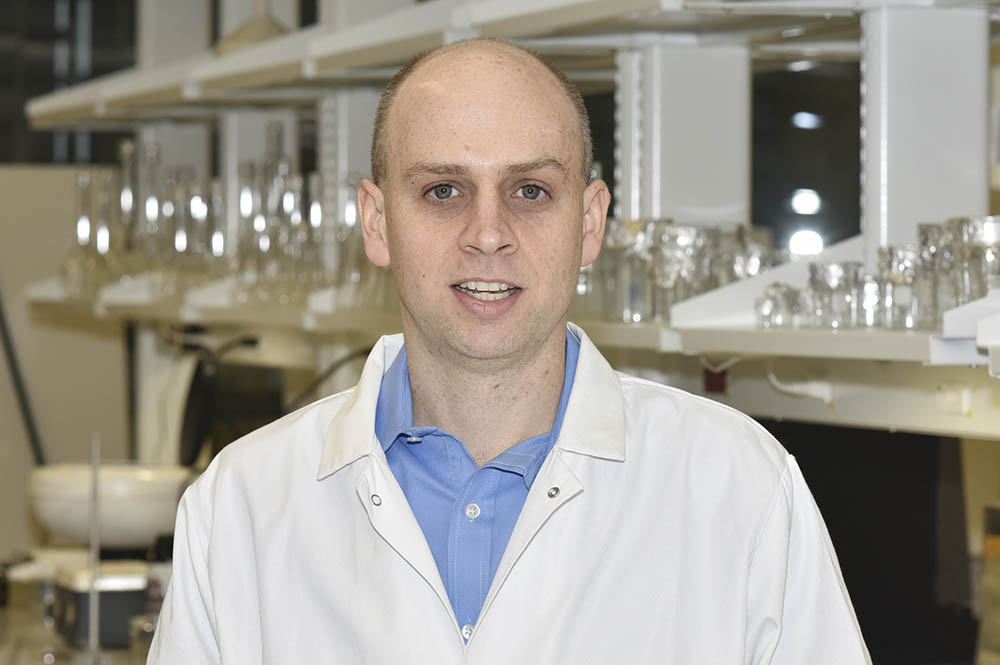
BIOE Assistant Professor Jenna Mueller
Throughout the past year, response to the COVID-19 crisis has demonstrated both the extraordinary power of science and the impact of health inequity on a global scale. But the disparities in health care access between high-income countries and low- and middle-income countries (LMICs) extend far beyond the scope of the current pandemic.
According to the World Health Organization (WHO), 4.8 billion people around the world currently lack access to safe, timely, and affordable surgical care and anesthesia, and the vast majority reside in LMICs.
“A majority of noncommunicable diseases – including almost all types of cancer – are treated with some sort of surgery,” said Fischell Department of Bioengineering (BIOE) Assistant Professor Jenna Mueller. “This isn’t a problem that’s going away. We have increasing numbers of noncommunicable diseases around the world. For example, cancer is on track to increase by 60 percent in the next 20 years alone.”
In LMICs, the prognosis is especially grim, as these countries account for nearly 70 percent of the world’s cancer-related deaths.
“One of the primary reasons for this disparity is that basic cancer diagnostics and treatment services are often inaccessible in low-income communities,” Mueller said.
According to the National Cancer Institute (NCI), as of January 2019, there were approximately 16.9 million cancer survivors in the United States. That number is projected to increase to 22.2 million by 2030. While this trend illustrates the rapid pace of advancement in cancer therapeutics, it is further buoyed by technological advances that make early detection and diagnosis possible. For example, cancers such as cervical, oral, breast, and colorectal cancers have high cure rates when detected and treated early.
But, early detection requires access to diagnostic technology – something many LMICs lack.
“Only 26 percent of LMICs report having pathology services available, which are needed to confirm disease and basically all types of cancer,” Mueller said. “And, only 30 percent report having treatment services available – like surgery and radiotherapy.”
Even in cases where diagnostics technology and treatment capabilities exist, there is an added challenge. In LMICs, up to 75 percent of patients who take part in a screening appointment do not return for subsequent visits, even after having a positive screen, Mueller said.
“There’s a profound need to have what’s called a ‘see and treat’ program, where patients could be both diagnosed and treated in the form of a single visit,” she said.
Recognizing this, Mueller and members of her Global Biomedical Devices Laboratory are taking a two-pronged approach toward addressing disparities in health care and cancer survival in order to better the odds of early diagnosis and treatment.
Mueller and her team’s first target is cervical cancer. Their aim is to develop a technique that would allow clinicians to host “see-and-treat” programs, whereby women could be treated as soon as precancerous cells are identified in the cervix.
Typically, cervical cancer is slow-growing – which means it is often curable with early diagnosis. And, detection is straightforward in high-income countries like the United States, where women with no history of cervical cancer are advised to have a Pap smear every three or five years, depending on their age and medical history. Within one to three weeks, pathology reports the results of the Pap smear to the patient’s doctor.
But, most LMICs lack the pathology force needed to process these otherwise simple tests.
“In Tanzania, for example, there is only one pathologist for every 2.5 million people,” Mueller said. “So, even if you do send something to a pathologist, you might not get results for six months to a year – if at all.”
Recognizing this challenge, Mueller and her research team are working to develop a technique that would enable doctors to screen a patient for cervical cancer and kill precancerous cells found in that same appointment. Existing methods such as cryotherapy – in which compressed gas and a metal probe are used to freeze lesions – require access to equipment that is difficult to transport and largely inaccessible in LMICs.
Instead, Mueller’s team is working on ethanol ablation, a technique in which ethanol is injected into diseased tissue to induce cell death. This technique is portable, highly accessible in LMICs, and has already been used to kill cells.
But, there are challenges.
Because of its low viscosity, ethanol has the propensity to leak into areas of the body adjacent to the lesion. To combat this, Mueller and her team added ethyl cellulose (EC) to the ethanol in order to increase the viscosity. Additionally, the researchers slowed the infusion rate of EC-ethanol delivery from a manual injection.
Studies of the Mueller Lab’s testing methods are promising. In hamster models, the ablation technique resulted in a complete regression of all tumors within seven days of treatment with EC-ethanol. Mueller received an NCI K99/R00 award to follow up on these promising initial results. Her current work focuses on optimizing EC-ethanol ablation to treat cervical pre-cancer.
“We are currently evaluating the safety and efficacy of EC-ethanol in a large animal model and have found that EC-ethanol is able to induce a clear ablation zone in a swine cervix with no side effects or adverse events,” Mueller said. We are following up on these exciting findings with the goal of moving into clinical studies in the future.”
Shifting gears, Mueller and her research team are increasing access to surgery from a second angle. Their aim is to create low-cost, portable surgical devices that improve access to surgery in LMICs and parts of the world that face health care disparities.
“In high-income areas of the United States, laparoscopic surgery is the standard of care for a variety of procedures within the chest and abdomen, many of which include cancer surgeries or excisions, as well as benign procedures,” Mueller said.
These types of surgeries are sought because they do not require large incisions and, instead, use a tiny camera and fine instruments manipulated through keyhole incisions. But, they require an operating room equipped with an expensive laparoscopic camera, viewing monitors, and additional tools – totaling upwards of $130,000 in initial purchases for each operating room, Mueller said.
In addition, current technology requires fragile fiber optic cables that need constant repair – which translates into expensive service contracts.
“But, patients in LMICs would benefit tremendously from laparoscopic surgery thanks to its advantages, which include smaller incisions, decreased pain, improved recovery time, fewer post-surgical infections, and shorter hospital stays,” Mueller said.
Recognizing this, Mueller and her team are working toward developing a low-cost, durable, and reusable laparoscope – called the ReadyView laparoscope – which requires less maintenance and can be easily sterilized. Their device prototype uses a color complementary metal-oxide-semiconductor (CMOS) detector and a ring of LEDs at the front of the device to decrease both costs and overall complexity of design, all while maintaining the image quality and resolution of a standard-of-care laparoscope. Even more, the device can be plugged into a laptop computer to display images, eliminating the need for expensive monitors and preventing loss of function during power outages.
“By taking advantage of advances in consumer grade electronics – like those we now have in our smart phones – and bringing them back into medical devices, we were able to substantially reduce the cost and complexity of the laparoscope,” Mueller said. “Our initial prototypes can be built for only $120 – nearly a 1,000-fold cost decrease compared with the standard-of-care device.”
Mueller traces much of her inspiration to her earlier work as both a student and a postdoctoral researcher at Duke University. During her time in Durham, she worked with a multidisciplinary team to develop the Pocket colposcope – a low-cost, portable device to screen women for cervical pre-cancer at the primary care setting. She and the team conducted studies to demonstrate the impact of the device on 1,000 women in eight countries. Together, they launched a company – Calla Health – at which Mueller works with industry partners to address feedback from the group’s studies.
“Getting to work on the Pocket colposcope and see it transform from an early prototype into a medical product that will be sold commercially by the end of 2021 has been one of the best learning experiences for me,” said Mueller. “And, it is one I hope to emulate with other technologies we are currently working on that are earlier in the translational pipeline.”
In the past month, Mueller received a grant and published two papers. The first paper – published in the Annals of Biomedical Engineering – described and characterized the initial prototypes of the ReadyView laparoscope. She recently received a grant through UM Venture’s Medical Device Development Fund to work with the University of Maryland’s Robert E. Fischell Institute for Biomedical Devices to develop second-generation prototypes that improve upon the original design. Mueller’s second paper – published in Global Health Science and Practice – explored the state of medical device regulation in the 14 member countries of the College of Surgeons of East, Central, and Southern Africa and South Africa. Mueller and her fellow co-authors are working to shed light on how a streamlined regulatory process across African nations would help drive medical device innovators to the African market, thereby increasing patient access to safe medical devices.
Mueller hopes to draw from her experiences to inspire others. Next fall, she will teach Engineering Design for Global Health, a bioengineering elective course that explores how the human-centered design framework can be applied to the development of new biomedical technologies to solve human health challenges.
“Human-centered design is an approach to problem solving that requires students to develop a deep understanding of the problem and engage with end users,” Mueller said. “One of the most exciting parts of the course is that students will get to learn about challenges in global health care directly from providers who work in LMICs. Watching students learn that they can apply bioengineering to increase access to health care in low-income communities is one of my favorite parts of being a professor.”
Full texts of the Annals of Biomedical Engineering paper and Global Health Science and Practice paper are available online. In addition to her BIOE appointment, Mueller also holds affiliations with the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center and the Robert E. Fischell Institute for Biomedical Devices.
Published April 5, 2021